Tips and resources to improve your mental health
Psychological Support
Understanding and Managing Anxiety
Topics covered on this page
What is anxiety?
Just as a cancer diagnosis and treatment affects your physical health, it can also affect how you feel, think, and go about your daily activities.
Anxiety or worry is a normal reaction when:
- Facing a threat or danger.
- Dealing with uncertainty or fear of the unknown.
- Feeling a lack of control over a situation or your body.
- Managing everyday stress.
When living with cancer you may find that anxiety becomes more intense at particular times, for example, when you are first diagnosed, when you are treated for cancer, or after completing your cancer treatment.
Certain situations can make these feelings worse such as waiting for test results or medical appointments. Occasionally, some cancer treatments and medications may have an effect on your body that can increase feelings of anxiety.
- Difficulties concentrating and focussing on tasks
- Thinking over and over about your cancer diagnosis and what the future will be like for you and your support persons
- Having a hard time getting certain thoughts out of your mind
- Feelings of worry or anxiety most of the day that do not go away
- Avoiding situations, people or things that make you anxious or trigger anxious feelings
- Withdrawing and not participating in daily tasks and social interactions with others
- Body tension
- Rapid heartbeat
- Increased sweating
- Dizziness
- Trembling
- Loss of appetite
- Nausea or other gut symptoms with no medical cause
- Difficulties sleeping
How can you manage anxiety?
There are a range of ways you can manage anxiety.
Anxiety is affected by how you think, which in turn affects how you feel and behave.
It can be helpful to become more aware of your anxiety provoking thoughts. Whenever you are feeling anxious:
- Stop and try to identify the thought that just passed through your mind.
- Write down your thoughts to identify any unhelpful patterns in your thinking. When you are feeling anxious you may have a tendency to make overgeneralisations, think of only the worst possible outcomes or to make assumptions about what another person is thinking. This kind of thinking can make your anxiety worse.
Sometimes when you are anxious you can overestimate the danger of a situation and underestimate your ability to handle it. It can help to think of different ways to look at a situation that is making you anxious, rather than jumping to the worst-case scenario.
People sometimes find that they are worrying for much of the day and night. To help with this, you may want to try ‘worry time’ to think about all of your concerns. Choose a set time each day to actively think about your concerns. You may even want to write them down. If you catch yourself worrying outside this time, write your worry down and remind yourself that you will have time to think about this concern during your worry time. This will help you to have more worry-free time and to gain a clearer picture of your situation.
A common cause of anxiety is not fully understanding cancer treatment or prognosis. Try to obtain the information you need from your treating team about the things that you do not completely understand. Ask lots of questions. Some people find it useful to write down the questions they may wish to ask.
Learning how to relax can reduce the impact of both anxiety and treatment-related symptoms (such as nausea). There are many different relaxation techniques. Two that you might want to try include:
Slow Breathing
- Slow breathing is a very effective way to become more relaxed.
- Simply breathe in slowly and deeply, all the way to your belly. Then let your breath out in a slow and controlled manner. Some people like breathing in through their nose, and out through their mouth. Do whatever is most comfortable for you.
- You can practice this regularly (10-15 minutes each day) to help with general relaxation and wellbeing.
Progressive Muscle Relaxation
This relaxation involves noticing tension in the muscles of your body, and relaxing this tension in each part of your body, one part at a time. Start with your head, and work ‘progressively’ through your arms, body, legs and feet. Repeat this as many times as needed.
Consider attending a relaxation or mindfulness meditation class or listening to an audio recording of a guided relaxation exercise.
Sometimes when we are feeling anxious we can neglect our physical health. Looking after our body can help with managing anxiety. You can improve your general health by:
- Decreasing caffeine and alcohol use
- Having a well-balanced diet
- Engaging in regular exercise
- Maintaining good quality sleep
If anxiety feels overwhelming and persists for a long time, it can be helpful to speak to a professional about how you are feeling. Explore your options listed at the bottom of this page.
Further information and support services
Further information- Beyond Blue - Anxiety information
- Black Dog Institute - Anxiety information
- Cancer Council - Emotions and Cancer booklet
You can begin by speaking to your General Practitioner (GP). GPs can discuss your emotional concerns with you and can link you to supports in the local community, such as a psychologist or social worker.
You can also speak to your cancer clinician. Most cancer services have a range of psychological support options including psychologists, social workers, psychiatric nurses and psychiatrists. If this isn’t available at your local health service, ask them what support is available in the local community.
You can find a local Psychologist with a referral or a mental health care plan from your GP.
- Search for a local Psychologist
- Search for a local Psychiatrist
- Health Direct
Health Direct provides information about what a mental health care plan is and how you can work with your GP to access a mental health care plan.
- This Way Up - Health anxiety course
This Way Up is a trusted Australian provider of evidence-based, internet-delivered Cognitive Behavioural Therapy (iCBT) programs.
- Moodgym
Moodgym is like an interactive self-help book which helps you to learn and practise skills which can help to prevent and manage symptoms of depression and anxiety.
- MindSpot - Mood mechanic course
A digital mental health clinic for all Australians.
- Mental Health Online - Anxiety Program
Mental Health Online provides comprehensive and effective online services and programs free of charge.
- Cancer Council NSW – Finding calm during cancer
Meditation and relaxation practices
- Headspace
Meditation and mindfulness app
- Smiling Mind
Web and app-based meditation program
- Cancer Council Victoria
A non-profit cancer charity organisation involved in cancer research, patient support, cancer prevention and advocacy.
- WeCan
A supportive care website
- Beyond Blue
All calls are with a trained mental health professional, and completely confidential. They will only ask you your first name and you can remain completely anonymous.
- Lifeline
Lifeline provides all Australians experiencing a personal crisis have access to 24-hour crisis support by trained professional
Body Image
What is body image?
Cancer and its treatments can affect how your body looks, feels and functions. This can lead to changes in your body image.
Your body image includes the way you see your body and how you think and feel about your body.
The way we look is often important to us and may also be linked to how we feel about ourselves.
Cancer and cancer treatment can cause a number of changes to your body.
Changes may include:
- Scars from surgery
- Hair loss due to chemotherapy or radiotherapy
- Hormonal changes
- Weight changes
- Loss of a body part
- Disfigurement
- Skin and tissue changes
- Adjusting to differences in how your body feels, moves and functions for example fatigue or loss of strength
- Sexual changes and feelings around intimacy
Some people find these physical changes lead to differences in the way they see their body and feel about their body. Some people feel more negatively towards their body. They may feel self-conscious about changes, or a loss of confidence in their body and what it can do or see their body as weak and vulnerable.
Others may experience changes to their body as positive. Positive changes may include a greater awareness and appreciation of your body and its abilities or greater motivation to look after yourself.
It is normal to feel:
- Anxious
- Less confident
- Angry
- Grief and loss about changes
- Sad or helpless
- Shocked and disappointed
- Or a combination of all of these emotions
- Some people with cancer feel they are no longer the person they used to be or worry about intimate and sexual relationships.
Changes in the way you think and feel about your body may also lead to changes in what you do, for example some people find themselves covering up parts of their body when they feel self-conscious or feel nervous about going out.
- Your body will take time to heal and recover from cancer treatment. Give yourself some time to adjust to changes and allow yourself to take it at your own pace
- Look after your body through eating well, exercising, sleeping and taking time to relax and engage in activities you enjoy
- Reach out and discuss changes and concerns with family and friends (your support team) as you will often find they can reassure you about how these changes may affect your relationship with them
- If you feel safe to do so share your worries about how you are looking and feeling with your intimate / sexual partner. In this way they will have some understanding of how you are feeling and can gain some understanding from your perspective of what is going on for you
- Reach out to other cancer survivors to share your experience and hear about other people’s experiences
- Try not to avoid looking at or dealing with body changes or activities such as going out, looking in the mirror or shopping for clothes. Avoiding these things may be a relief in the short term, but it may make things more difficult in the long term. Everyone will have an individual response and you will know when you are ready to make this step
- It can be helpful to remind yourself of other important parts of your life and unique aspects of your personality as a whole. We often tie our appearance to our identity, so it is important to remember that we have our own strengths and desirable qualities that continue to exist even in the face of changes to our appearance
It may be important to speak to your doctor, nurse or social worker about changes you are experiencing and how they can support you. Discussing how to take positive action can be empowering. Health services may have resources available to support people undergoing body changes, including wig services and scalp cooling.
You may also find you would like support from a mental health professional to work through any changes and how you feel about them. Explore your options listed at the bottom of this page.
Further information and support services
Further information- Look good feel better
- Cancer Council NSW – Changed body image information
- University Health Network (Canada) - Managing Body Image Concerns After Cancer Treatment Booklet
- Cancer Council Victoria – Hair loss information
You can begin by speaking to your General Practitioner (GP). GPs can discuss your emotional concerns with you and can link you to supports in the local community, such as a psychologist or social worker.
You can also speak to your cancer clinician. Most cancer services have a range of psychological support options including psychologists, social workers, psychiatric nurses and psychiatrists. If this isn’t available at your local health service, ask them what support is available in the local community.
You can find a local Psychologist with a referral or a mental health care plan from your GP.
- Search for a local Psychologist
- Search for a local Psychiatrist
- Health Direct
Health Direct provides information about what a mental health care plan is and how you can work with your GP to access a mental health care plan.
- Cancer Council NSW – Finding calm during cancer
Meditation and relaxation practices
- Headspace
Meditation and mindfulness app
- Smiling Mind
Web and app-based meditation program
- Cancer Council Victoria
A non-profit cancer charity organisation involved in cancer research, patient support, cancer prevention and advocacy.
- WeCan
A supportive care website
- Beyond Blue
All calls are with a trained mental health professional, and completely confidential. They will only ask you your first name and you can remain completely anonymous.
- Lifeline
Lifeline provides all Australians experiencing a personal crisis have access to 24-hour crisis support by trained professional
Depression
What is depression?
Cancer and its treatment can affect your mood and the way you feel about yourself. Feelings of sadness, shock and grief are normal responses to the diagnosis and treatment of cancer and will be experienced by most people with cancer at different times. You may adjust to these changes in your own time and at your own pace.
Depression however is more than just a low or blue mood. It is a serious illness that affects a person’s quality of life, relationships, thinking and physical health.
People who experience both depression and cancer often feel distressed, tend to have trouble completing everyday tasks and may find it difficult to follow medical advice.
It is often difficult to diagnose depression in people with cancer because the physical symptoms of depression can overlap with cancer symptoms and the side effects of cancer treatment. It is important when speaking to your doctor to also describe and talk about what you are thinking and feeling.
- Ongoing sadness or low mood for most of the day
- Feeling close to tears or experiencing intrusive or continual crying
- Feeling ‘numb’ or not feeling anything much at all
- Feelings of helplessness, or hopelessness
- Feelings of guilt or worthlessness
- Difficulties concentrating, remembering and making decisions
- Loss of interest or pleasure in most activities that you used to enjoy
- Unintentional weight loss or weight gain
- Loss of energy or fatigue
- Loss of sexual interest
- Difficulty going to sleep, early waking, sleeping too much, or lying awake for hours
- Feeling restless, irritable or agitated
- Being slowed down enough for others to notice
- Thoughts of self-harm, thoughts that the life you have is not worth living or wishing you were dead
What situations and events increase your risk of developing depression?
- Loss of physical abilities
- Poorly controlled pain
- Recurrence of cancer
- Poor cancer prognosis
- Advanced stage of cancer
- Additional medical problems
- Lack of family / friend / carer support
- Unemployment
- Past history of depression
- Family history of depression or suicide
- Previous suicide attempts
- Drug or alcohol abuse
How can you manage depression?
There are a range of ways depression can be managed:
- Self-management strategies (e.g. lifestyle changes and self-help strategies)
- Psychological therapies (e.g. cognitive behavioural therapy, interpersonal psychotherapy)
- Medical management (e.g. medications)
If you feel depressed what can you do?
It is important that you seek information about your cancer from your treating team. Inform them of any changes in your level of pain or other physical symptoms. Your treating team may help you to better understand your cancer. They may be able to assist you with better symptom management which in turn may improve your mood.
Depression may be affected by how we think, which in turn affects how we feel and behave.
People who are depressed often have a number of unhelpful thinking patterns about themselves, their relationships and their situation. It may be helpful to keep a journal of your thoughts and identify what could be a trigger to these thoughts. Understanding your thinking patterns can help change the way you experience your situation.
Planning can be helpful. You may feel uncertain about planning too far in advance. Try to make a list of what you will do tomorrow and each day of the following week. Each day mark off your list of achievements. Reschedule the tasks you have not completed for the next day. Keeping a list of tasks will help you concentrate your thoughts beyond what you are experiencing in this minute and help you focus on other thoughts.
Do something nice for yourself every day such as spending time reading, having a special treat, visiting a local café for a hot drink, walking to a local park, listening to music, speaking to a friend, day -dreaming of a past holiday or any other activities that you enjoy.
Learning how to relax can help people manage low mood and treatment related symptoms (such as pain).
There are many different relaxation techniques. Two that you might want to try include:
Slow Breathing
- Slow breathing is a very effective way to become more relaxed.
- Simply breathe in slowly and deeply, all the way to your belly. Then let your breath out in a slow and controlled manner. Some people like breathing in through their nose, and out through their mouth. Do whatever is most comfortable for you.
- You can practice this regularly (10-15 minutes each day) to help with general relaxation and wellbeing.
Progressive Muscle Relaxation
This relaxation involves noticing tension in the muscles of your body, and relaxing this tension in each part of your body, one part at a time. Start with your head, and work ‘progressively’ through your arms, body, legs and feet. Repeat this as many times as needed.
Consider attending a relaxation or meditation class or listening to an audio recording of a guided relaxation exercise
Improving your general health by engaging in regular exercise such as a short walk around the block or to the local cafe, having a well-balanced diet, maintaining good quality sleep and reducing caffeine/alcohol use can all assist in managing depression.
Seek social support and speak about how you are feeling. Support can assist people in coping with difficult situations and helps them feel less isolated.
If your depression symptoms persist for a long time (more than 2 weeks), it can be helpful to speak to someone professional about how you are feeling. Explore your options listed at the bottom of this page.
Further information and support services
Further information- Beyond Blue - Depression information
- Black Dog Institute - Understanding depression information
You can begin by speaking to your General Practitioner (GP). GPs can discuss your emotional concerns with you and can link you to supports in the local community, such as a psychologist or social worker.
You can also speak to your cancer clinician. Most cancer services have a range of psychological support options including psychologists, social workers, psychiatric nurses and psychiatrists. If this isn’t available at your local health service, ask them what support is available in the local community.
You can find a local Psychologist with a referral or a mental health care plan from your GP.
- Search for a local Psychologist
- Search for a local Psychiatrist
- Health Direct
Health Direct provides information about what a mental health care plan is and how you can work with your GP to access a mental health care plan.
- Moodgym
Moodgym is like an interactive self-help book which helps you to learn and practise skills which can help to prevent and manage symptoms of depression and anxiety.
- This Way Up online depression course
This Way Up is a trusted Australian provider of evidence-based, internet-delivered Cognitive Behavioural Therapy (iCBT) programs.
- Mental Health Online - Depression Program
Mental Health Online provides comprehensive and effective online services and programs free of charge.
- Black Dog Institute iBobbly app
A social and emotional wellbeing self-help app for young Aboriginal and Torres Strait Islander peoples aged 15 years and over.
- Cancer Council NSW – Finding calm during cancer
Meditation and relaxation practices
- Headspace
Meditation and mindfulness app
- Smiling Mind
Web and app-based meditation program
- Cancer Council Victoria
A non-profit cancer charity organisation involved in cancer research, patient support, cancer prevention and advocacy.
- WeCan
A supportive care website
- Beyond Blue
All calls are with a trained mental health professional, and completely confidential. They will only ask you your first name and you can remain completely anonymous.
- Lifeline
Lifeline provides all Australians experiencing a personal crisis have access to 24-hour crisis support by trained professional
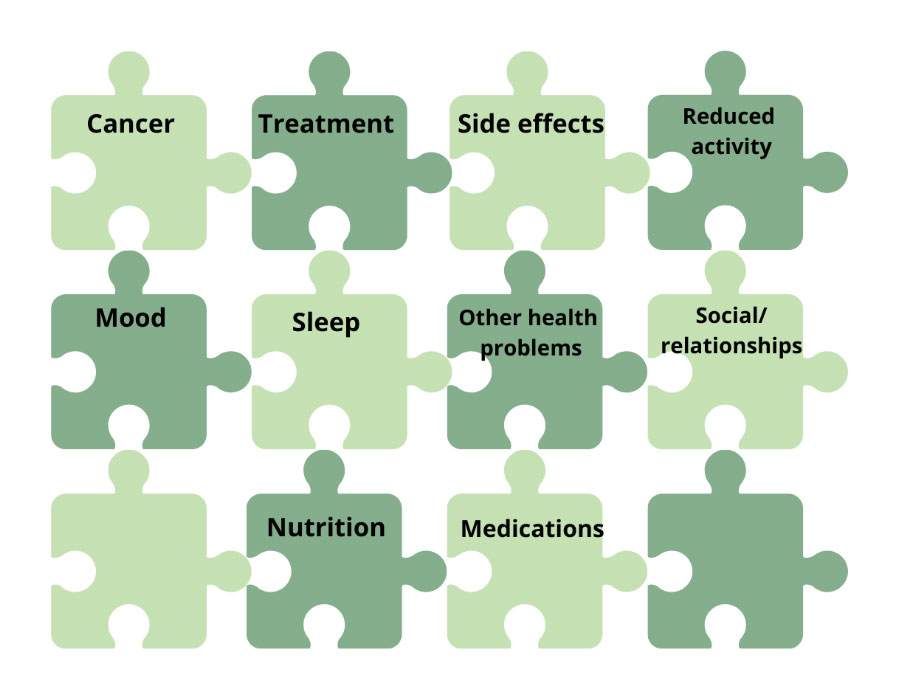
Fatigue
What is fatigue?
Fatigue is a feeling of tiredness, or lack of energy.
Unlike everyday tiredness, fatigue in cancer is a different experience:
- Sleep is not so refreshing
- Your body feels different
- Your thinking may be affected e.g. concentration, memory, planning
- Everyday tasks may be more difficult to do
- These effects can cause you frustration, despair and worry.
Fatigue is common during and after cancer surgery, treatments and medications. It can happen to anyone, but it may be reduced or prevented.
You can watch this video to learn more about cancer-related fatigue.
People who have:
- Fatigue before starting treatment
- Depression or sleep problems
- Multiple or long-term health problems
- Low physical activity or fitness
What can you do to lower your fatigue?
Increase your energy supply by:
- Doing physical activity such as housework and exercise as it may help to reduce or prevent fatigue.
- Start with what you can easily do. If you have not been active previously, ask your doctor for an exercise referral to a Physiotherapist and or Exercise Physiologist
- Find a form of exercise you enjoy – walking/ swimming/ walking in water/ riding a bike, moving to music, Tai Chi
- Pace yourself!
- Slowly increase the time and intensity of exercise so you feel a bit puffed
- Start with 5 minutes and increase slowly by 5 minutes each day towards a goal of 30 minutes a day.
- Keep doing your usual activities, as much as you can without getting too tired and taking breaks. For example, if you are cleaning – clean one room at a time and return to complete the next area after you have had sufficient rest (replenish your energy)
- Eat foods that have good energy and protein.
- Cut up your ingredients for dinner, have a rest and then return to cook the food
- If you are mowing the lawn, do one section or area at a time. It is about planning and managing your energy level.
View this video resource for more information: Doc Mike Evans – a short cancer fatigue overview video
- Ask your General Practitioner or cancer clinician for help with your tiredness
- Check for other conditions you may have that can also cause fatigue
- Learn to work with the energy you have
- Do not push yourself to exhaustion
Increase your energy:
- Many people find an individual or group exercises or support program helps
- Sometimes you will become more motivated to participate in exercise if you are with others. For example, walking to the local café/park/beach with a support person, walking groups, or scheduled exercise classes
View the video resources listed below for more information:
- Peter MacCallum Cancer Centre – Session on managing cancer-related fatigue
- Alberta Health Services – Living well with cancer-related fatigue
- Alberta Health Services – Exercise for cancer-related fatigue
- University of Michigan Comprehensive Cancer Center – Nutrition for cancer fatigue
- Alberta Health Services – Pacing yourself with cancer-related fatigue
- See your General Practitioner to check for health conditions that may add to your fatigue
- See an occupational therapist for help managing day-to-day activities
- See a psychologist to manage the mental and emotional aspects of fatigue
Use energy saving methods:
- Do things more slowly, for shorter times
- Plan your day to include rest and activity
Increase your energy:
- A dietitian can help you to improve your nutrition with healthy foods
- An exercise specialist can help you to build your strength and energy with an exercise program
View this video resource for more information: Mayo Clinic – 9 ways to manager your cancer fatigue
Many health conditions can cause or add to fatigue. See your GP to check health conditions that may add to your fatigue:
- Ongoing pain, low mood (depression), stress (anxiety) and sleep problems
- Taking medications that cause drowsiness
- Having infections, viruses or low red blood cells
- Dehydration (not drinking enough water)
- Other health conditions
Further information and support services
Further information- Australian Cancer Survivorship Centre - Dealing with cancer-related fatigue fact sheet
- Cancer Council Victoria - Fatigue and cancer information
You can begin by speaking to your General Practitioner (GP). GPs can discuss your emotional concerns with you and can link you to supports in the local community, such as a psychologist or social worker.
You can also speak to your cancer clinician. Most cancer services have a range of psychological support options including psychologists, social workers, psychiatric nurses and psychiatrists. If this isn’t available at your local health service, ask them what support is available in the local community.
You can find a local Psychologist with a referral or a mental health care plan from your GP.
- Search for a local Psychologist
- Search for a local Psychiatrist
- Health Direct
Health Direct provides information about what a mental health care plan is and how you can work with your GP to access a mental health care plan.
- Untire app
Untire gives you the tools to reduce cancer fatigue and get back to living life.
- Cancer Council podcast - Managing Cancer Fatigue
- Cancer Council NSW – Finding calm during cancer
Meditation and relaxation practices
- Headspace
Meditation and mindfulness app
- Smiling Mind
Web and app-based meditation program
- Cancer Council Victoria
A non-profit cancer charity organisation involved in cancer research, patient support, cancer prevention and advocacy.
- WeCan
A supportive care website
- Beyond Blue
All calls are with a trained mental health professional, and completely confidential. They will only ask you your first name and you can remain completely anonymous.
- Lifeline
Lifeline provides all Australians experiencing a personal crisis have access to 24-hour crisis support by trained professional
Fear of Recurrence
What is fear of cancer recurrence?
Fear of cancer recurrence is the fear or worry that cancer could return or spread in the same place or any other part of the body.
Fear of cancer recurrence affects most people after finishing cancer treatment.
It is normal and understandable to be worried about your cancer coming back or progressing.
The diagram below shows common features of fear of cancer recurrence.
- Further treatment
- Further disability, pain or suffering
- Impact on quality of life
- Being unable to fulfil obligations
- Impact of a recurrence on loved ones
- Loss and grief about not being able to live out lifetime goals
- The possibility of death and the process of dying
- Follow-up appointments or scans
- Physical symptoms or changes
- Anniversaries of major cancer events such as diagnosis
- Hearing about cancer stories in the news, celebrities, or other people’s cancer experience
- Seeing others who have cancer and having treatment when you go for appointments
If your fear of cancer recurrence is high, you may have intrusive thoughts or images about the cancer returning or progressing.
- You may be very alert and looking out for physical symptoms
- You might notice aches, pains and changes in how you feel or look
- You might check physical symptoms excessively or avoid symptom monitoring
- You might notice a lot of anxiety about tests, scans, treatment, or medical appointments
These concerns may impact daily life and cause a lot of distress or anxiety for people with high levels of fear of cancer recurrence.
If you are worried about cancer returning or progressing, what can you do?
You might write them down or tell them to a friend or family member. Remind yourself that it’s very normal and understandable to be worried about your cancer coming back or progressing.
Be aware of times when your fear will be higher and plan how you will manage your fears at that time. For example, when you have an upcoming scan, you might write your worries down, do things that are important to you, practice your relaxation, and make sure you eat and sleep well.
Write a list of questions for your cancer team.
Ask your doctors what symptoms you need to watch out for, how to check symptoms (if applicable), and how/when to respond to new symptoms. Try to keep to their guidelines, and remind yourself that not all physical symptoms are signs of cancer.
Do things that are important to you, even if you are feeling fearful or worried.
People around you might not want to tell you they are also worried about the possibility of your cancer returning or progressing. Let them know how you’re feeling and that you’d just like them to listen and hear your concerns.
Do regular relaxation such as calming breathing, or mindfulness meditations. Try to do 5-15 minutes of relaxation each day and immediately when you are having thoughts of recurrence.
Avoid foods or drinks that increase your anxiety such as caffeine or alcohol. Continue exercising as you usually do. Try to keep to healthy sleep habits.
It can be helpful to speak to a mental health professional about how you are feeling. Explore your options listed at the bottom of this page.
Further information and support services
Further information- Cancer Council - Living Well After Cancer booklet
- Cancer Council NSW - Fear of the cancer returning information
- Australian Cancer Survivorship Centre - Coping with Fear of your Cancer Coming Back fact sheet
- Macmillan (UK) - Worrying about Cancer Coming Back booklet
You can begin by speaking to your General Practitioner (GP). GPs can discuss your emotional concerns with you and can link you to supports in the local community, such as a psychologist or social worker.
You can also speak to your cancer clinician. Most cancer services have a range of psychological support options including psychologists, social workers, psychiatric nurses and psychiatrists. If this isn’t available at your local health service, ask them what support is available in the local community.
You can find a local Psychologist with a referral or a mental health care plan from your GP.
- Search for a local Psychologist
- Search for a local Psychiatrist
- Health Direct
Health Direct provides information about what a mental health care plan is and how you can work with your GP to access a mental health care plan.
- Cancer Council NSW – Finding calm during cancer
Meditation and relaxation practices
- Headspace
Meditation and mindfulness app
- Smiling Mind
Web and app-based meditation program
- Cancer Council Victoria
A non-profit cancer charity organisation involved in cancer research, patient support, cancer prevention and advocacy.
- WeCan
A supportive care website
- Beyond Blue
All calls are with a trained mental health professional, and completely confidential. They will only ask you your first name and you can remain completely anonymous.
- Lifeline
Lifeline provides all Australians experiencing a personal crisis have access to 24-hour crisis support by trained professional
Grief
What is grief?
Grief is the process of responding to a loss and it can affect all parts of your life. It is not just an emotion in the context of death and dying.
With a cancer diagnosis, grief can happen shortly after diagnosis, during treatment and beyond.
There are both tangible and intangible losses.
Tangible losses may include losses or changes to your:
- Body parts ( e.g. loss of body parts, disfigurement, loss of hair)
- Function (e.g. ability to work, or engage in normal activities)
- Finances (e.g. loss of job, change in financial security)
- Relationships (e.g. change in roles in relationships or intimacy)
- Possessions (e.g. accommodation, housing)
Intangible losses may include losses or changes to your:
- Independence
- Identity
- Time and energy levels
- Future events, goals and plans that you once looked forward to
- Career aspirations
How can grief impact you?
Grief is a very individual process. There is no right way to grieve.
Everyone’s grief is shaped by their gender, personality, family and cultural background, and life experience.
Grief is not the same as depression nor does is it occur in phases or stages. There is no set timeline for grief.
After a loss you can experience a range of intense emotions.
These may include:
- Shock
- Disbelief
- Guilt
- Blame
- Numbness
- Anger
- Resentment
- Irritability
- Longing
- Sadness
- Relief
- Anxiety
- Panic
Grief can lead to:
- Rumination where you go over and over your loss
- Difficulties concentrating
- Difficulties making decisions
- Difficulties remembering things
- Confusion
Grief can feel like you are losing control of your mind.
Common thoughts associate with grief may include:
- “I’ll never get over this”
- “I can’t cope”
- “This is not fair”
Grief can lead to:
- Changes in sleep patterns
- Changes in appetite
- Dizziness, headaches, muscle aches, nausea
- Pain
- A generally unwell feeling
- Exhaustion and fatigue
- Crying
- Keeping busy or the opposite – loss of interest in usual activities
- Snapping or feeling impatient with others
- Talking about the loss or avoiding it
- Withdrawal from friends and family
What can you do to help with the grief process?
Although the sadness of loss may never go away completely, most people will cope with grief and loss through the support of their family and friends and not require counselling or medication.
- Look after your physical health through exercise, a healthy diet and by limiting alcohol
- Establish a routine
- Give yourself time to grieve
- Spend time with people that you find supportive and share with them how you are feeling. Talk about the loss. Avoidance can lead to feeling isolated.
- Keep a diary. Write down how you feel about the grief and loss. Write down your memories and observations
- Give yourself permission to do things that you enjoy or that can distract you. Start doing pleasant things again. This might include doing some gardening, going to a movie, doing a puzzle, playing a board game, eating out or any other activity that you enjoy
For the loss of a loved one:
- It might help to write a goodbye letter. In the letter you might want to share: how saying goodbye makes you feel, your memories, what you miss, and how you will remember them
- Share your memories of your loved one
- Join a bereavement group
Further information and support services
Further information- Cancer Council Victoria – Understanding grief booklet
- Cancer Council - Coping with Grief Podcast
- Headspace – Understanding grief and loss fact sheet
- National Association for Grief and Loss
- Australian Centre for Grief and Bereavement
You can begin by speaking to your General Practitioner (GP). GPs can discuss your emotional concerns with you and can link you to supports in the local community, such as a psychologist or social worker.
You can also speak to your cancer clinician. Most cancer services have a range of psychological support options including psychologists, social workers, psychiatric nurses and psychiatrists. If this isn’t available at your local health service, ask them what support is available in the local community.
You can find a local Psychologist with a referral or a mental health care plan from your GP.
- Search for a local Psychologist
- Search for a local Psychiatrist
- Health Direct
Health Direct provides information about what a mental health care plan is and how you can work with your GP to access a mental health care plan.
- Cancer Council NSW – Finding calm during cancer
Meditation and relaxation practices
- Headspace
Meditation and mindfulness app
- Smiling Mind
Web and app-based meditation program
- Cancer Council Victoria
A non-profit cancer charity organisation involved in cancer research, patient support, cancer prevention and advocacy.
- WeCan
A supportive care website
- Griefline
Skilled telephone counsellors are available 6am to midnight, 7 days a week.
- The Compassionate Friends Victoria
24/7 grief-support phone line provided by trained peer-support volunteers
- Beyond Blue
All calls are with a trained mental health professional, and completely confidential. They will only ask you your first name and you can remain completely anonymous.
- Lifeline
Lifeline provides all Australians experiencing a personal crisis have access to 24-hour crisis support by trained professional
Pain
Topics covered on this page
What is Pain?
Many people with cancer experience pain at some point in time. It may be caused or related to the cancer itself or its treatments including chemotherapy, radiotherapy or surgery.
Experiencing pain can have a range of impacts including physical (reduced mobility, sleep, energy) and emotional (low mood, worry, doing fewer pleasurable activities).
How can you manage pain?
It is important to involve your medical team in the management of your pain to target the biological aspects of pain (for example with medication). Let you doctors and treating team know about your pain throughout your cancer treatment.
The good news is there are also things you can do to help manage your pain. This includes learning to think differently about pain, doing more of the things that are important to you, and learning how to build up your activity levels.
Notice when your thoughts about pain have become extreme and may be unhelpful (e.g. “I’ll never achieve anything with this pain”). Try to rephrase these thoughts so that they are more realistic (e.g. “I notice the pain right now, but also know I can still do some of the things that are important to me”).
Focus on your other sensations by noticing 5 things you can see, 5 things you can hear, 5 things you can smell and 5 other (pleasant and/or non-painful) sensations you can feel.
Try to make time to do small things that you enjoy. Plan for this in advance and schedule this in. If it helps, involves significant others including friends or family members in your plans.
- Add in rest periods
- Build up slowly. Do not do more activity than you have planned, even on a good day
- If you have a bad day, try to keep to your plan but be kind to yourself
- If your pain flares up, go back one level and pace back up again
- Reward yourself when you achieve small steps or goals
Where can you get additional help?
Speak to your treating doctor. You may wish to consider accessing additional support from allied health services including psychologists or physiotherapists to help manage your pain. Your doctor will be able to speak with you about how this applies to you.
Further information and support services
Further information- Cancer Council Victoria - Overcoming cancer pain booklet
- Cancer Council Victoria - Frequently asked questions about cancer pain
- American Society of Clinical Oncology (ASCO) - Managing cancer-related pain guide
You can begin by speaking to your General Practitioner (GP). GPs can discuss your emotional concerns with you and can link you to supports in the local community, such as a psychologist or social worker.
You can also speak to your cancer clinician. Most cancer services have a range of psychological support options including psychologists, social workers, psychiatric nurses and psychiatrists. If this isn’t available at your local health service, ask them what support is available in the local community.
You can find a local Psychologist with a referral or a mental health care plan from your GP.
- Search for a local Psychologist
- Search for a local Psychiatrist
- Health Direct
Health Direct provides information about what a mental health care plan is and how you can work with your GP to access a mental health care plan.
- This Way Up - Chronic pain course
This Way Up is a trusted Australian provider of evidence-based, internet-delivered Cognitive Behavioural Therapy (iCBT) programs.
- MindSpot - Pain course
A digital mental health clinic for all Australians.
- Cancer Council podcast - The thing about cancer – Managing cancer pain
- BBC podcast: You me and the big C – Managing the pain (UK)
- Cancer Council NSW – Finding calm during cancer
Meditation and relaxation practices
- Headspace
Meditation and mindfulness app
- Smiling Mind
Web and app-based meditation program
- Cancer Council Victoria
A non-profit cancer charity organisation involved in cancer research, patient support, cancer prevention and advocacy.
- WeCan
A supportive care website
- Beyond Blue
All calls are with a trained mental health professional, and completely confidential. They will only ask you your first name and you can remain completely anonymous.
- Lifeline
Lifeline provides all Australians experiencing a personal crisis have access to 24-hour crisis support by trained professional
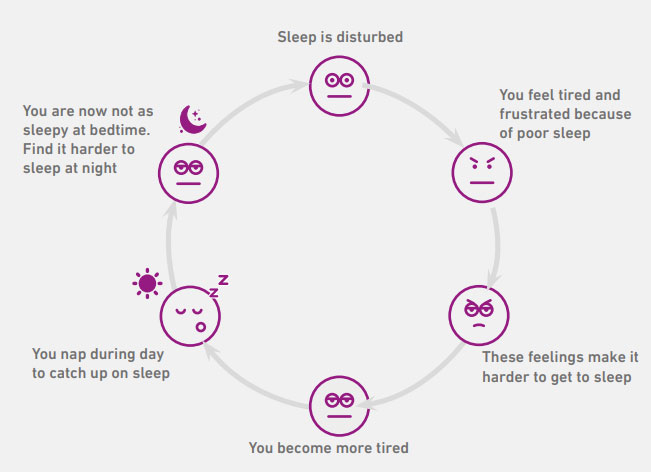
Sleep Problems
Why is sleep important?
We all need to sleep. Sleep is an important part of:
- Restoring our energy
- Repairing our bodies
- Processing information to learn new things
Each night you cycle through different types of sleep, including:
- Light and drowsy sleep
- Deep sleep that restores our energy
- “Rapid Eye Movement” sleep, when dreams occur
You cycle through these different types of sleep, and it is normal to wake briefly a number of times throughout the night.
It is also normal to experience times when you don’t get enough sleep. This might be because your sleep is disrupted by life situations like noise, shift work, parenting responsibilities, or health issues (such as when you have cancer and go through treatment).
When you have poor sleep you can experience a range of problems such as:
- Low energy and fatigue
- Poor concentration and memory
- Irritability
- Tearfulness
- Lower tolerance for pain and stress
- Difficulty managing anxiety or low mood
How does cancer impact sleep?
It is very common for sleep to be disrupted by:
- Cancer
- Cancer treatments
- Treatment side effects like pain, hot flushes and nausea.
Cancer and its treatment demands can also disrupt our sleep by increasing:
- Anxiety
- Worrying
- Stress
- Grief
- Sadness
- Other emotional difficulties
Consider talking to your General Practitioner (GP) or oncology team if you are having problems sleeping. It is often possible to treat sleep problems, or better manage side-effects that are disrupting sleep.
How can you sleep better?
Our bodies are really good at catching on sleep when we have experienced some sleep disruption.
However, it is important to make sure that you are giving yourself the best chance to regain a good sleep pattern.
Here are some common causes of sleep problems that you might need to address:
Try to get up at the same time each day. This will help your body clock know when to wake up and when to sleep.
Try to eat a well-balanced diet and at regular times, and not in the hours before bed.
Avoid caffeine (e.g. tea/coffee), energy drinks, and other stimulants like nicotine in the evenings.
Avoid too much alcohol at night, especially just before bed. They can be relaxing, but actually make the quality of sleep very poor.
In the evening, only do activities that are calming and help you wind down (e.g. listening to music, audiobooks, or a meditation).
Exercise in the daytime (not before bed) helps you to build a drive for sleep.
Avoid daytime napping, or if you must nap, try to nap at a regular time and briefly (e.g. 30 minutes)
In the evenings, reduce the light in your room (e.g. have only one small lamp on and try not to use bright screens).
Try not to do other activities in bed, you want your body to associate bed with sleep.
Don’t miss good opportunities of sleepiness in evening. Similarly, don’t lie in bed for long periods of time if you’re not sleepy, stay up and do relaxing activities until you feel sleepy.
Explore ways to reduce stress and improve your mood (e.g. self-care, seeking support from family or friends, speaking to a therapist). Helping yourself to be in a good emotional state can improve sleep.
What are unhelpful thoughts about sleep?
Some thoughts and beliefs we have about sleep can make it even harder to fall asleep. If you are saying stressful things to yourself about sleep (e.g. “I’m never going to get to sleep”, or “This is going to ruin my day tomorrow”), you might need to catch these and change those thoughts to something more helpful, like:
- “Peaceful rest is also good for me.”
- “Sleep problems are normal.”
- “This won’t last forever.”
- “If I don’t sleep very well tonight, I’ll catch up on sleep tomorrow.”
What should you do if you can’t sleep?
If you are trying to sleep for 20-30 minutes and still feel awake (i.e. not sleepy or drowsy), it is often best to stop trying to sleep. This can make you frustrated, which makes it more difficult to sleep. Instead, you can:
- Get out of bed, and leave the bedroom if you can
- If you are worried about a specific problem, write down one positive action you can do tomorrow to address it (e.g. ask someone for advice)
- Try to stay in low lighting and avoid using bright screens
- Do something quiet and relaxing (e.g. calming music, reading, meditation)
- Notice yourself becoming more relaxed and sleepy, and go back to bed when ready
What else can help?
This is one of the best treatments for night time sleep problems and can be accessed by seeing a Psychologist.
There are a number of medications that may help with sleep, you can discuss with your treating doctor or GP.
Examples of over-the-counter sleep aides are anti-histamines, valerian, chamomile, lavender, and certain vitamins. Discuss with treating doctor if you plan to try these to ensure there is no conflict with any treatment medications.
Further information and support services
Further information- Peter MacCallum Cancer Centre - Can-Sleep Self-Help Booklet
- Better Health Channel - Sleep hygiene information
- Breast Cancer Network Australia (BCNA) – Sleepless nights: Breast cancer and sleep fact sheet
- AYA Cansleep booklet
You can begin by speaking to your General Practitioner (GP). GPs can discuss your emotional concerns with you and can link you to supports in the local community, such as a psychologist or social worker.
You can also speak to your cancer clinician. Most cancer services have a range of psychological support options including psychologists, social workers, psychiatric nurses and psychiatrists. If this isn’t available at your local health service, ask them what support is available in the local community.
You can find a local Psychologist with a referral or a mental health care plan from your GP.
- Search for a local Psychologist
- Search for a local Psychiatrist
- Health Direct
Health Direct provides information about what a mental health care plan is and how you can work with your GP to access a mental health care plan.
- This Way Up - Insomnia course
This Way Up is a trusted Australian provider of evidence-based, internet-delivered Cognitive Behavioural Therapy (iCBT) programs.
- SleepHub podcast - Sleep and Cancer
- Cancer Council NSW – Finding calm during cancer
Meditation and relaxation practices
- Headspace
Meditation and mindfulness app
- Smiling Mind
Web and app-based meditation program
- Cancer Council Victoria
A non-profit cancer charity organisation involved in cancer research, patient support, cancer prevention and advocacy.
- WeCan
A supportive care website
- Beyond Blue
All calls are with a trained mental health professional, and completely confidential. They will only ask you your first name and you can remain completely anonymous.
- Lifeline
Lifeline provides all Australians experiencing a personal crisis have access to 24-hour crisis support by trained professional
Stress Management
Topics covered on this page
What is stress?
Stress is the body’s reaction to pressure from an event or situation. You may notice you experience stress as a physical, mental or emotional reaction. Stress affects all of us and is not the same as anxiety or depression but can be a factor in increasing your risk to developing psychological problems.
A diagnosis of cancer, upcoming tests, or medical appointments are understandable causes of stress.
Whilst stress is a normal human reaction, at times it can feel overwhelming, so learning ways to manage stress can be helpful.
Stress can be acute (in the moment) or chronic (long lasting). If the effects of stress stay in your body for too long it can have a damaging effect. Being aware of the warning signs can be important.
- Headache
- Problems with sleeping (too much or too little)
- Muscle stiffness and tension (jaw clenching, neck pain)
- Gastrointestinal problems
- Change in sex drive
- Increased blood pressure
- Feeling stuck
- Desire to smoke
- Up and down mood
- Anxiety
- Restlessness
- Feeling unmotivated
- Irritability
- Agitation
- Short temper/quick to anger
- Crying
- Panic attacks
- Persistent low mood
- Worrying all the time
- Feeling you’re under constant pressure
- Drinking or taking drugs to deal with your stress
- Overeating
- Withdrawing from family and friends
Strategies to cope with stress
- What are your realistic concerns?
- Do you need to ask for more information from your treating team, or need details of a treatment plan?
- What areas of your life are affected by your diagnosis?
- Is there additional support I can utilise? (e.g. financial, burdens of childcare, domestic responsibilities)
Stress is normal at times of great change or trying to adjust to new information or physical changes. Be kind and compassionate to yourself.
- Who are you able to share your concerns with?
- Are there family, friends, colleagues you can talk to about how you are feeling?
Some behaviours, such as drinking alcohol or smoking, may give us short-term relief, but can actually increase our stress over the longer-term. When you get the urge to engage in these behaviours try choosing another activity, such as exercise or a relaxation practice, which may be more helpful.
Physical activity may help increase the production of endorphins (happy hormones) helping us feel better, as well as reducing the negative effects of stress.
Your distress and fitness level can be improved with almost any form of exercise. The most important thing is to pick an activity that you enjoy, and is easy to access.
The practice of focused attention has been found to reduce the stress response. Guides or classes for meditation are available through a number of providers. Explore the relaxation and mindfulness resources listed at the bottom of this page.
Sleep allows our brains to recharge and our bodies to rest. Sometimes physical discomfort or worry can interfere with our ability to get to sleep or stay asleep. We know that prioritising sleep, and reducing behaviours that negatively impact sleep (e.g. caffeine intake) significantly affects our stress response.
Eating regularly and a well-balanced diet are important ways of managing stress.
When life is difficult it is important that you take time out to engage in activities that you enjoy, and remind yourself of what you value and what makes you happy.
If your stress is interfering with your ability to function and is ongoing, you may want to find a mental health professional. Explore your options listed at the bottom of this page.
Further information and support services
Further information- Beyond Blue – Reducing stress information
- National Cancer Institute – Stress fact sheet
You can begin by speaking to your General Practitioner (GP). GPs can discuss your emotional concerns with you and can link you to supports in the local community, such as a psychologist or social worker.
You can also speak to your cancer clinician. Most cancer services have a range of psychological support options including psychologists, social workers, psychiatric nurses and psychiatrists. If this isn’t available at your local health service, ask them what support is available in the local community.
You can find a local Psychologist with a referral or a mental health care plan from your GP.
- Search for a local Psychologist
- Search for a local Psychiatrist
- Health Direct
Health Direct provides information about what a mental health care plan is and how you can work with your GP to access a mental health care plan.
- Cancer Council NSW – Finding calm during cancer
Meditation and relaxation practices
- Headspace
Meditation and mindfulness app
- Smiling Mind
Web and app-based meditation program
- Cancer Council Victoria
A non-profit cancer charity organisation involved in cancer research, patient support, cancer prevention and advocacy.
- WeCan
A supportive care website
- Beyond Blue
All calls are with a trained mental health professional, and completely confidential. They will only ask you your first name and you can remain completely anonymous.
- Lifeline
Lifeline provides all Australians experiencing a personal crisis have access to 24-hour crisis support by trained professional
Scanxiety
Topics covered on this page
What is scanxiety?
Scanxiety is the nervousness and dread that you may experience before, during and while waiting for results.
Scans are associated with:
- The trauma of diagnosis
- Fear of cancer returning or progression
- A change in therapeutic approach
- Discomfort and confinement
How can you manage scanxiety?
- Know your own signs of scanxiety
- Label it and acknowledge it as scanxiety
- See the people you like –if possible, avoid other stressful situations
- Do regular exercise, meditation and relaxation
- Eat a healthy diet. Sugar and caffeine will make anxiety worse
- Prepare yourself with information you need for the scan, such as a referral letter or fasting requirements
- Wherever possible schedule your scan in the morning for fewer delays
- Bring along a support person
- Use distraction. Try to focus on something else such as trying to list all the movies you saw in the last year or remembering family members birthdates
- Practice meditation
- Medication can help
- Talk to the technician about your anxiety
- Do things you enjoy (make plans and keep busy)
- Talk to your support persons or cancer support groups
- Meditate and practice relaxation
- Help someone else out. Helping others makes us feel good about ourselves
- Use helpful self-talk (Try not to predict the outcome, remind yourself that you are resilient and that you can cope)
Further information and support services
Further information- PanCare Foundation: Managing cancer scanxiety article
- Melanoma Patients Australia: Scanxiety article
You can begin by speaking to your General Practitioner (GP). GPs can discuss your emotional concerns with you and can link you to supports in the local community, such as a psychologist or social worker.
You can also speak to your cancer clinician. Most cancer services have a range of psychological support options including psychologists, social workers, psychiatric nurses and psychiatrists. If this isn’t available at your local health service, ask them what support is available in the local community.
You can find a local Psychologist with a referral or a mental health care plan from your GP.
- Search for a local Psychologist
- Search for a local Psychiatrist
- Health Direct
Health Direct provides information about what a mental health care plan is and how you can work with your GP to access a mental health care plan.
- Cancer Council NSW – Finding calm during cancer
Meditation and relaxation practices
- Headspace
Meditation and mindfulness app
- Smiling Mind
Web and app-based meditation program
- Cancer Council Victoria
A non-profit cancer charity organisation involved in cancer research, patient support, cancer prevention and advocacy.
- WeCan
A supportive care website
- Beyond Blue
All calls are with a trained mental health professional, and completely confidential. They will only ask you your first name and you can remain completely anonymous.
- Lifeline
Lifeline provides all Australians experiencing a personal crisis have access to 24-hour crisis support by trained professional
Wellbeing
Topics covered on this page
Sleep
We have an internal body clock that is set to various routines and external triggers like sunshine. Learn to work with your body clock. Set up habits that promote good sleep.
- Get up at the same time every day
- Go to bed at the same time – consistency builds quality
- Build a ritual around sleep to train yourself, for example check phone for the last time, read for 20 minutes, tidy your room, stretch, meditate, sleep… whatever suits you
Anything you can do to make your room quieter, darker or more comfortable will help, but of course it isn’t always easy, but at least think about:
- Right temperature – and the right clothes for you
- Dark – close the curtains, or even cover the window if you can
- Quiet – if you need to use ear plugs
And also beware of alcohol – whilst it may relax you, it will also wear off in the middle of the night and wake you to go to the toilet
Try anything that will calm you down – relaxation exercises, reading, a warm bath… anything you find helpful to wind down
And avoid social media or work in bed – it fires up your brain
For further information, visit the Sleep page.
Nutrition
Cancer requires special attention to nutrition. Consider seeing a Dietitian for tailored nutrition advice (speak to a healthcare professional at your local health service or medical practice to arrange a referral).
Healthy eating advice for the general population is outlined in the tips below. This does not replace specific advice provided by your healthcare professional.
Enjoy a wide variety of nutritious food from the five food groups every day:
- Vegetables
- Fruit
- Wholegrains, such as breads, cereals, rice, pasta, noodles, polenta, couscous, oats, quinoa and barley
- Lean meats, poultry, fish, eggs, tofu, nuts, seeds and legumes/beans
- Dairy foods such as milk, yoghurt, cheese (and/or alternatives)
- It is best to limit your intake of foods containing added sugars, saturated fat and added salt.
Drink less alcohol. For further details, visit alcohol.gov.au
Avoid too much caffeine such as coffee, tea, energy or cola drinks.
For further information, visit the Cancer Council Victoria’s nutrition page
Exercise
Before taking part in any exercise program, either during or soon after your treatment, it is important to talk with your oncologist or general practitioner (GP) about any precautions you should take.
Consider seeing an Exercise Physiologist or Physiotherapist for tailored advice (speak to a healthcare professional at your local health service or medical practice to arrange a referral).
Exercise advice for the general population is outlined in the tips below. This does not replace specific advice provided by your healthcare professional.
- Exercise is the cheapest and easiest way to improve your mental health
- Exercise helps with anxiety, depression, stress levels as well as having physical benefits
- The trick is building a routine – finding ways to incorporate some exercise each day – even as little as 20 minutes helps
- Try to find a mix of activities such as walking, cycling, running, swimming, gym or community sport
- Consider things you haven’t tried before for example, yoga or pilates. There are many online options you can do in your own home, such as Yoga for Beginners
For further information, visit the Cancer Council Victoria’s exercise page
You may also like to join Peter MacCallum Cancer Centre’s online ‘Let’s talk exercise’ program with a qualified exercise physiologist.
Stress
There are two secrets to reducing stress:
- The first is to learn relaxation strategies
- The second is to find structured approaches to dealing with stressful situations
For relaxation strategies, think of relaxation like any other skill – you have to learn it and practice it to get good at it. To really improve your relaxation skills, you should try to do at least 20 minutes practice per day.
A structured approach to dealing with stress means finding simple ways to contain your worries. The most common is to write down the problem causing stress, then write a list of possible things you can do, and for each thing, write down the pros and cons. Then allow yourself time to think about the information, and then make a plan.
Explore the relaxation and mindfulness resources listed at the bottom of this page.
For further information, visit the Stress Management page.
Relationships
Great relationships are the final step in developing psychological wellbeing.
- Think about the relationships that nourish you and nurture them
- Think of the relationships that cause you stress, and consider pulling away for a short time until you feel stronger
- Re-connect with people from your past who you miss – a simple phone call or email can do wonders “Hi, it’s me, I was thinking about you and thought I’d call and say hi”
For the problematic relationships, start to actively think about how you could improve them. Start with small changes, and see how you go.
- Effective communication – honesty is always best. Never underestimate kindness in interactions. Listen, not to comment, but to truly understand. If people feel heard, they are more willing to meet you halfway
- Schedule time to talk – when you’re both calm and free of distractions
- Don’t take other people’s anger personally – in 99% of cases, they are just stressed and letting off steam. However, you should never tolerate violence or aggression
- Schedule time for fun things
- Respect other people’s boundaries and protect your own – tolerate time apart and try not to live in each other’s pockets, especially during times of isolation when you are stuck in the house together
- State the problem
- Truly attempt to understand the other person‘s perspective
- Engage in discussion
- Listen as much as you talk
- Don’t rush it
- Be optimistic
- Be kind
- Be creative and bold
- Make contact but don’t expect too much too soon – often the other person needs a little time
- Remember that initiating repair is a form of love
If you have the energy and space, think about your friends and family who might benefit from some connection and initiate contact.
Writing with Cancer program
The Writing with Cancer program is a collaboration with a professional writer and person of lived experience, Catherine Deveny and the Psychology and Psychiatry Departments at Peter MacCallum Cancer Centre. There are 6x 40 minute videos which focus on expressive writing tasks, psychoeducation and the opportunity for reflection and guided emotional “check-in”.
The aims are:
- To improve psychological wellbeing
- To learn about writing
- To facilitate creative, self-expression and enjoyment.
Watch the series:
Further information and support services
Finding a mental health professionalYou can begin by speaking to your General Practitioner (GP). GPs can discuss your emotional concerns with you and can link you to supports in the local community, such as a psychologist or social worker.
You can also speak to your cancer clinician. Most cancer services have a range of psychological support options including psychologists, social workers, psychiatric nurses and psychiatrists. If this isn’t available at your local health service, ask them what support is available in the local community.
You can find a local Psychologist with a referral or a mental health care plan from your GP.
- Search for a local Psychologist
- Search for a local Psychiatrist
- Health Direct
Health Direct provides information about what a mental health care plan is and how you can work with your GP to access a mental health care plan.
- Cancer Council NSW – Finding calm during cancer
Meditation and relaxation practices
- Headspace
Meditation and mindfulness app
- Smiling Mind
Web and app-based meditation program
- Cancer Council Victoria
A non-profit cancer charity organisation involved in cancer research, patient support, cancer prevention and advocacy.
- WeCan
A supportive care website
- Beyond Blue
All calls are with a trained mental health professional, and completely confidential. They will only ask you your first name and you can remain completely anonymous.
- Lifeline
Lifeline provides all Australians experiencing a personal crisis have access to 24-hour crisis support by trained professional
Privacy Policy
Information for statistical purposes
Unless this website asks for specific personal information, Peter MacCallum Cancer Centre will only collect information relating to your use of the website for statistical purposes to assist Peter MacCallum Cancer Centre in improving users’ experience of the site. Such information may include the:
- date and time of your visit
- pages accessed and documents downloaded
- referring site
- type of browser you are using
Google Analytics
Our website uses Google Analytics, a service which transmits website traffic data to Google servers in the United States. Google Analytics does not identify individual users or associate your IP address with any other data held by Google. We use reports provided by Google Analytics to help us understand website traffic and webpage usage.
By using this website, you consent to the processing of data about you by Google in the manner described in Google’s Privacy Policy-and for the purposes set out above.
Security of personal information
Peter MacCallum Cancer Centre takes reasonable steps to protect the personal information it holds from misuse and loss, and from unauthorised access, modification or disclosure.
While Peter MacCallum Cancer Centre endeavours to provide a secure online environment through its website, you should be aware that there are inherent risks associated with the transmission of information via the internet.
Where personal information is no longer needed for the purpose for which it was collected, Peter MacCallum Cancer Centre will take reasonable steps to destroy or permanently de-identify such personal information.
Third party sites
Any links on this website to a third-party site are provided for convenience only and a link to a third party site is not an endorsement by Peter MacCallum Cancer Centre. Peter MacCallum Cancer Centre is not responsible for the content and privacy policies of other sites, and recommends that you review each site’s privacy policy.
Cookies
Peter MacCallum Cancer Centre’s website may use cookies to enhance some website functionality.
Cookies work by placing some information on your computer that is accessed by the website whenever you visit the site. In effect, the cookie helps the website “remember” you when you return to the site.
Internet browsers generally allow an individual to control whether they will accept cookies from a website. Individuals who choose not to accept cookies will still be able to access Peter MacCallum Cancer Centre’s website, but the user may notice that some website functions do not work properly or efficiently.
Enquiries and feedback
If you have any queries about Peter MacCallum Cancer Centre’s privacy policy or if you have any complaint about the handling of your personal information, contact Peter MacCallum Cancer Centre’s Patient Liaison Officer via switchboard on (03) 8559 5000.
Disclaimer
This content contains information that has been approved by reference groups comprising relevant health professionals, consumers and non-government organisations.
Content is sourced from published research literature, grey literature sources (e.g. clinical guidelines) and opinions of clinical experts. It is not intended to reflect all of the available evidence and is not intended to be exhaustive.
The authors acknowledge that it is possible that other relevant guidelines or scientific findings may have been published since the development of the website.
Acknowledgments
Screening tool references
Kessler-10
Kessler, R.C., Barker, P.R., Colpe, L.J., Epstein, J.F., Gfroerer, J.C., Hiripi, E., Howes, M.J, Normand, S-L.T., Manderscheid, R.W., Walters, E.E., Zaslavsky, A.M. (2003). Screening for serious mental illness in the general population Archives of General Psychiatry. 60(2), 184-189.
Distress thermometer
Adapted from the National Comprehensive Cancer Network (NCCN) Distress Thermometer. Available from: https://www.nccn.org/docs/default-source/patient-resources/nccn_distress_thermometer.pdf?sfvrsn=ef1df1a2_4
Contact
For questions or comments related to this website, please email CancerMindCare@petermac.org. To contact the Peter MacCallum Cancer Centre Psychology Department please call 03 8559 5220.